Vaccine-preventable diseases still exist throughout the world, even in the U.S. While you might not see some of these diseases every day, they are still common in other countries and could easily be brought into the U.S.
If we stopped vaccinating, the relatively small number of cases we have in the U.S. could very quickly become tens or hundreds of thousands of people infected with diseases. Even if your family does not travel internationally, you and your family could come into contact with travelers anywhere in your community. When people don’t receive all of the recommended vaccinations and are exposed to a disease, they can become seriously sick and spread it through their community.
The only vaccine-preventable disease that is completely eradicated (gone) from the world is smallpox. Polio is now the next closest to being eliminated around the world, but it still exists in some countries including Afghanistan and Pakistan. Since we know that diseases can spread from country to country through international travelers and trade, we must all continue to be vaccinated so the disease doesn’t come back in the U.S.
All vaccine-preventable diseases are not the same. Some diseases are more deadly, and some others are more contagious. But whether the chance of getting sick or dying from is a particular disease is 1 in 100 or 1 in 10,000, you must decide if the risk is worth taking with your family’s and community’s health. No one ever thinks that they or their child will be the 1 in 10,000 that will die from a vaccine-preventable disease.
How can I protect my family and my community from vaccine-preventable diseases?
To best protect yourself and every member of your family from vaccine-preventable diseases, follow the CDC’s recommended immunization schedules. Vaccines are not just for protecting ourselves and our families. They also protect the people of all ages in our community who are unable to get certain vaccines; who are too young to get vaccinated against certain diseases; who might have failed to respond to a vaccine; or who might be particularly susceptible to serious diseases and their complications for other reasons like cancer or HIV. This concept is known as “community immunity” or “herd immunity”.
Vaccines also protect our children’s children and their children by keeping diseases that used to be more common in the U.S. from coming back. If we stopped vaccinating in the U.S., we could find ourselves fighting serious and often deadly diseases we thought we had gotten rid of (or were mostly gone) decades ago.
What disease outbreaks have happened recently in the United States?
COVID-19
COVID-19 is a disease caused by a coronavirus called SARS-CoV-2.
On January 30, 2020, the World Health Organization (WHO) declared a global health emergency and on March 13th, the United States declared a national emergency.
Since the pandemic began, there have been over 100 million cases of COVID-19 and over 1,225,657 due to COVID-19 in the U.S. For the most up-to-date tracking of COVID-19 cases and related hospitalizations and deaths, visit the COVID Tracker.
For more about COVID-19 and the vaccines developed to protect against it, visit our COVID-19 page.
Pertussis (Whooping Cough)
Whooping cough (also known as pertussis) is a common disease in the U.S. that may cause serious illness in people of all ages and can even be life-threatening, especially in babies. Before the vaccine was routinely used in the U.S., whooping cough was one of the most common childhood diseases and a major cause of childhood death.
While the number of whooping cough cases has gone down since the vaccine, frequent outbreaks still happen in the U.S. and around the world. In 2024, reported cases of whooping cough increased across the U.S., indicating a return to pre-pandemic patterns. More than six times as many cases were reported at the end of 2024, compared to the same time in 2023. Learn more about whooping cough outbreaks.
Sadly, up to 20 babies still die each year in the U.S. due to whooping cough. More than half of babies younger than 1 year old who get whooping cough need treatment in the hospital. The younger the baby is when he or she gets whooping cough, the more likely he or she will need to be treated in a hospital.
It may be hard for you to know if your baby has whooping cough because many babies with this disease don’t cough at all. Instead, it can cause them to stop breathing and turn blue. In other people with whooping cough, they might cough, but it may not have the “whoop” sound.
The best way to prevent whooping cough is through vaccination – DTaP is the vaccine for babies and children. Tdap is the vaccine for preteens/teens, adults and pregnant women.
To best prevent whooping cough in newborns, medical and public health experts recommend that pregnant women receive the Tdap vaccine during the third trimester (between the 27th and 36th week of pregnancy) of every pregnancy. (The American College of Obstetricians and Gynecologists and the American College of Nurse-Midwives support this recommendation.)
Through Tdap vaccination, a pregnant woman’s body will create protective antibodies and pass some of them to her baby before birth, providing the baby with short-term protection against whooping cough until he or she is old enough to start getting his own whooping cough (DTaP) vaccinations. Parents should also ask all family members, friends and caregivers who will be around their baby to get vaccinated against the disease. It takes approximately two weeks after getting the vaccine to be protected from the disease.
Learn more about whooping cough and the vaccines that help protect against it in our Vaccines and Diseases section.
View more stories from families affected by whooping cough.
Hear how whooping cough may sound in children and adults.
Measles
Measles is still a common disease in many parts of the world including some countries in Europe, Asia, the Pacific and Africa. Every year, unvaccinated travelers (Americans or foreign visitors) get measles while they are in other countries and bring measles with them into the U.S. They then spread the disease to other people who are not protected against measles. Outbreaks usually occur in communities with groups of unvaccinated people.
Between December 1, 2023 and January 23, 2024, the Centers for Disease Control and Prevention (CDC) was notified of 23 confirmed U.S. cases of measles, including seven direct importations of measles by international travelers and two outbreaks with more than five cases each.
So far in 2025, measles cases in the U.S. are already more than double last year. As of April 5, 2025, a total of 636 confirmed measles cases were reported by 22 jurisdictions: Alaska, California, Colorado, Florida, Georgia, Kansas, Kentucky, Maryland, Michigan, Minnesota, New Jersey, New Mexico, New York City, New York State, Oklahoma, Rhode Island, Tennessee, Texas, Vermont, and Washington.
Of these 636 cases, almost all were unvaccinated, or vaccination status was unknown. Cases have been predominately in people 5–19 years of age and children under 5 years old. Experts warn the number of true measles cases could be much larger due to the confusion and delay in the outbreak response.
74 patients have been hospitalized for measles complications. The age group with the highest rates of hospitalizations from this measles outbreak is children under the age of 5.
There have been 3 deaths from measles in 2025, tragedies we have not seen in the U.S. in decades. An unvaccinated adult in New Mexico and 2 healthy, unvaccinated young girls in Texas have died from measles due to this outbreak. The passing of these girls marks the first death from measles in a child in the U.S. since 2003.
Learn more about the current measles outbreaks.
Only the fact that most people in the U.S. are vaccinated against measles prevents these clusters of measles cases from becoming serious epidemics.
Measles is one of the most contagious diseases known to humans. It spreads through the air when a person with measles coughs or sneezes, and can linger in the air and on surfaces for up to 2 hours. It is so contagious that if 1 person is infected, 9 out of 10 people around him or her will also become infected if they are not protected.
Measles is more than just a rash and a fever. It can lead to serious illness and health complications, even death.
People at the most risk of complications include children under 5 years old, adults over 20 years old, pregnant women, and people with weakened immune systems.
- About 1 out of 5 people who get measles will be hospitalized.
- As many as 1 out of every 20 children with measles gets pneumonia, the most common cause of death from measles in young children.
- Measles may cause pregnant women who have not got the MMR vaccine to give birth prematurely, or have a low-birth-weight baby.
The MMR vaccine is the best way to protect against measles. Before the measles vaccine was routinely used in the U.S., about 3 to 4 million people got measles each year, and of those people, 400 to 500 died and 8,000 were hospitalized.
- Children need 2 doses of MMR vaccine – the first dose between 12 -15 months of age and the second dose between 4-6 years old.
- Adults who were born during or after 1957 (and don’t have evidence of immunity against measles) should get at least 1 dose of MMR vaccine. Certain adults may need 2 doses of MMR. Ask your healthcare provider.
- If your family is traveling internationally, the recommendations for MMR vaccine are a little different. Before leaving the country, babies 6 through 11 months old should get 1 dose of MMR vaccine, and children 12 months of age or older need 2 doses of MMR vaccine (separated by at least 28 days). Teens and adults who do not have evidence of immunity should get 2 doses of MMR vaccine (separated by at least 28 days).
Learn more about measles and the MMR vaccine in our Vaccines and Diseases section.
Mumps
Mumps is a contagious disease that can be spread when infected people cough, sneeze or talk. Since the mumps vaccine is not used everywhere, it is a common disease in many countries including the United Kingdom, which has had several mumps outbreaks since 2004, and Japan, which does not routinely vaccinate against mumps. According to CDC, the U.S. saw a range of different mumps outbreak settings from 2015 to 2017. Cases started to increase in late 2015, and between January 2016 and June 2017, 150 outbreaks (9,200 cases) were reported. Many of the cases occurred in close-knit communities in New York City and Arkansas, on different college campuses across the country, and within the National Hockey League (NHL). Cases also occurred in households, schools, church groups, workplaces, and large parties and events. Most recently, in 2024, a total of 357 mumps cases were reported. As of March 27, 2025, 23 jurisdictions reported a total of 67 mumps cases. Learn more about current mumps outbreaks in the U.S.
The MMR vaccine is the best way to protect against mumps. During a mumps outbreak, public health authorities might recommend an additional dose of MMR vaccine for people who belong to groups at increased risk for getting mumps. Your local public health authorities or institution will notify you if you are at increased risk and should receive this additional dose. Learn more about mumps and the MMR vaccine in our Vaccines and Diseases section.
Meningitis
Cases of meningococcal disease* (often referred to as meningitis) still occur in the U.S., and although rare, outbreaks also happen. The onset of an outbreak is unpredictable and the consequences are often devastating. Outbreaks occur in communities, schools, colleges, prisons and other populations. According to the National Meningitis Association:
- Approximately 600 – 1,000 people get meningococcal disease in the U.S. each year.
- 21% of all meningococcal disease cases occur in preteens, teens and young adults ages 11 to 24 years old.
Meningococcal disease is a rare, and sometimes deadly, bacterial infection that can strike and progress very quickly (sometimes within hours). It is not easy to recognize meningococcal disease since the signs and symptoms can resemble flu or other viral infections, and it can lead to terrible complications such as hearing loss, brain or kidney damage, or limb amputations, and even death in 10-15 percent of cases.
Since meningococcal infection is hard to identify and can progress rapidly, prevention is very important. The best way to protect against meningococcal disease is vaccination. There are a few vaccines that offer protection from various strains of meningococcal disease – find the latest recommendations here.
In addition to routine recommendations, the CDC recommends vaccinating people identified as being at increased risk during a meningococcal outbreak.
Learn more about meningococcal disease and the vaccines that protect against it in our Vaccines and Disease section.
Influenza (flu)
Although it’s not usually called an outbreak, the CDC estimates that flu leads to:
- Between 9 million and 41 million illnesses every year
- Between 140,000 and 710,000 hospitalizations every year
- Between 12,000 and 52,000 deaths every year
In addition, each year in the U.S., more than 20,000 children under the age of 5 are hospitalized and over 100 children die. In the 2024–25 flu season, over 150 children have died from flu and its complications. Most were not fully vaccinated.While flu infection rates dropped following the outbreak of COVID-19 (likely due to the impacts of social distancing) they have rebounded in recent years to pre-pandemic levels.
Flu is caused by viruses that infect the respiratory tract (nose, throat and lungs). Flu spreads through the air when people cough or sneeze and people nearby inhale the virus. Flu viruses can also be spread to adults and children when a person wipes their eyes or puts their hands in their mouth or nose after touching a surface that has flu virus on it.
Serious complications of flu can result in hospitalization or death, even in healthy people.
Many children, teens and adults – including pregnant women – are at high risk for flu and its dangerous complications.
For the best protection against flu, the CDC recommends that everyone over 6 months of age receive a flu vaccine every year. It takes 2 weeks for the vaccine to provide you with immunity, so you want to make sure you and your family are protected with the vaccine at least 2 weeks before the flu begins spreading in your community.
There are many benefits of flu vaccination:
- Flu vaccination can keep you from getting very sick with flu.
- Flu vaccination can reduce your risk of being hospitalized due to flu.
- Flu vaccination can be lifesaving in children.
- Vaccination helps protect pregnant individuals during and after pregnancy and can protect the baby from flu illness for several months after birth.
Visit our Personal Stories section to read stories from individuals and families who were affected by serious flu complications.
Human Papillomavirus (HPV)
Although not usually referred to as an outbreak, HPV is so common that most people – about 1 in 4 – will get an HPV infection at some point in their lives. More than 40 million people in the U.S. are currently infected with HPV and about 13 million people in the U.S., including teens, become infected with HPV each year.
Every year in the United States, HPV causes 37,800 cancers in men and women. HPV vaccination is cancer prevention. In fact, HPV vaccination can prevent 90% of these cancers, and genital warts, from ever developing.
The CDC recommends that all children 11-12 years old get 2 doses of HPV vaccine. The vaccine offers the greatest health benefits those who receive both of the recommended doses before having any type of sexual activity.
Some parents may be surprised to learn that sexual intercourse is not necessary for infection. Oral-genital and hand-genital transmission of some genital HPV types is possible. A person can become infected during their first sexual encounter.
Before being licensed in the U.S., the HPV vaccine was studied very carefully for safety and effectiveness, and it continues to be monitored by CDC and FDA. With over 120 million doses of HPV vaccine distributed in the U.S., backed by over 12 years of monitoring and research, no serious safety concerns have been linked to HPV vaccination. Scientific studies continue to show that HPV vaccines are safe and effective. Learn more.
Learn more about HPV and the vaccine to help protect against HPV infection and HPV-related cancers.
View personal stories from people who were diagnosed with HPV-related cancers.
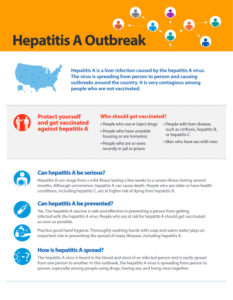
Hepatitis A
Hepatitis A is a serious disease of the liver caused by the hepatitis A virus. It can range in severity from a mild illness lasting a few weeks to a severe illness lasting several months.
Hepatitis A is usually spread by contact with people who are infected with the virus, or from contact with objects, food, water or drinks contaminated by the feces of an infected person, which can easily happen if someone doesn’t properly wash his or her hands after using the toilet.
According to the CDC, there are widespread outbreaks of hepatitis A across the U.S. – mostly among people who use drugs and people experiencing homelessness. Since the hepatitis A outbreaks were first identified in 2016, 37 states have reported:
- 44,937 cases
- 27,461 hospitalizations
- 424 deaths
Visit the CDC’s website for the latest information on hepatitis A outbreaks in the U.S. and additional information for healthcare providers.
The hepatitis A vaccine is the best way to prevent hepatitis A infection. Learn more about hepatitis A and the vaccine that protects against it.
Download CDC’s Hepatitis A fact sheet.