Human Papillomavirus (HPV)
What is HPV?
Human papillomavirus (HPV) is a common virus that can lead to six types of cancer: cervical, vaginal, vulvar, anal, penile, and oropharyngeal (throat) cancer. HPV is also a major cause of genital warts.
HPV is so common that nearly all sexually active men and women will be infected with the virus at some point in their lives. HPV can be passed even when an infected person has no signs or symptoms.
In most cases, HPV resolves on its own, and many people never realize they were infected. However, the virus can remain in the body for weeks or even a lifetime. For some individuals, genital warts may develop, and in some cases, the infection can lead to cancer over time.
Learn about one woman’s battle with HPV-related cancer here.
On this page you will find:
people in the U.S. are currently infected with HPV, and about 13 million new infections, including among teens, occur each year.
How does HPV spread?
The virus spreads through intimate skin-to-skin contact, including vaginal, anal, or oral sex with someone who has the virus, even if they don’t show any signs or symptoms.
However rare, there have been instances where HPV has been passed to the baby during childbirth when the mother has an active case of genital warts. If this happens, the baby usually clears the virus on their own. In rare cases, the baby may develop warts in its throat, which will require surgery to prevent the warts from blocking the baby’s airway. In most cases if the mother has HPV-related cervical cancer, the baby can be delivered safely.
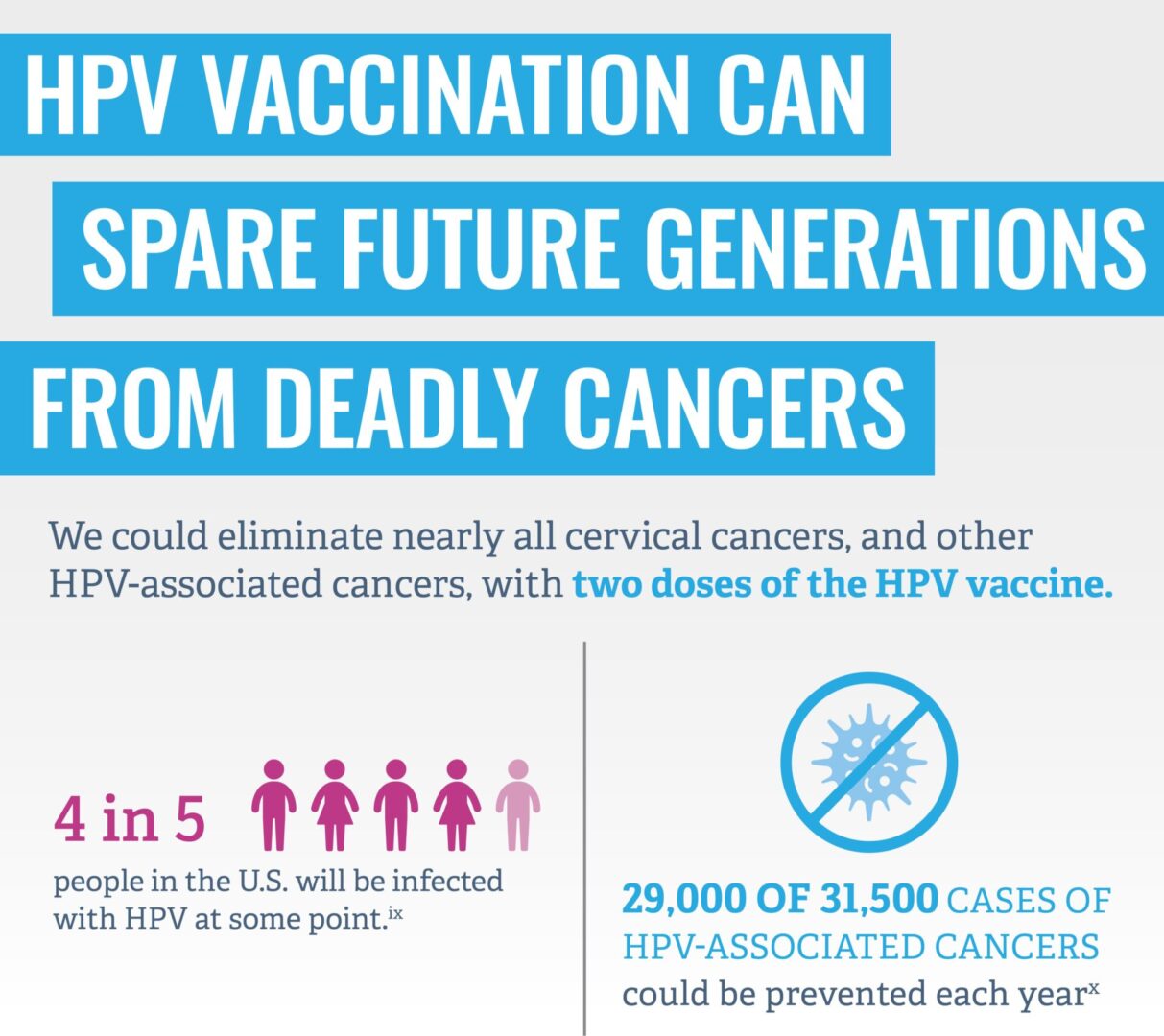
HPV can affect anyone. Approximately 40 million people in the U.S. are currently infected with HPV, and about 13 million new infections, including among teens, occur each year.
How common is HPV-related cancer in the US?
According to CDC, every year in the United States, HPV causes 36,500 cancers in men and women. That’s the same as the average attendance for a baseball game! The HPV vaccine could prevent approximately 90% of these cancers from ever developing, but only if given before people become exposed to the virus.
HPV can spread without symptoms.
Even when the infected person has no symptoms, the virus can still be transmitted.
What are the symptoms of HPV?
Genital warts typically appear as small bumps or clusters of bumps in cauliflower-like shape in the infected area. These may grow into large clusters in someone with a weakened immune system. A healthcare provider can usually diagnose them through a visual examination.
HPV-related cancers often don’t cause symptoms making it especially important for women to get regular Pap tests to screen for cervical cancer, in addition to receiving the HPV vaccine.
Currently, there is no routine screening test for other HPV-related cancers, so it’s crucial to visit your doctor regularly for checkups and get vaccinated to help prevent these cancers from developing.


How can I prevent HPV?
HPV vaccination is cancer prevention. HPV vaccination helps prevent six types of cancers caused by HPV in both men and women. HPV vaccination can also help prevent genital warts.
There is currently one licensed HPV vaccine for use in the United States called Gardasil 9. Gardasil 9 protects against 9 types of cancer-causing HPV types: 6, 11, 16, 18, 31, 33, 45, 52, and 58.
For maximum cancer prevention, it is important to be vaccinated before first exposure to the virus.


Preteens and Teens
The American Academy of Pediatrics recommends starting the HPV vaccination series at age 9. For adolescents under 15, two doses of the vaccine are needed to achieve maximum cancer prevention benefits. The vaccine is most effective when given before age 13, as it triggers the strongest immune response. Delaying vaccination beyond this age can reduce the level of cancer protection.
For children aged 9–12, the HPV vaccination schedule consists of two doses:
- 1st dose: Given at age 9–12 years
- 2nd dose: Administered 6–12 months after the first dose
If children aged 9–14 receive their two doses less than 5 months apart, a third dose will be required to ensure full protection. Teens and young adults who start the HPV vaccination series between 15 and 26 years old will need three doses of HPV vaccine.
- The doses are given over 6 months.
- If your teen isn’t vaccinated yet, talk to their doctor about doing so as soon as possible.


Adults
HPV vaccination is recommended for everyone through age 26, if not already vaccinated.
Adults aged 27 through 45 who have not yet received the vaccine should consult with their healthcare provider to assess their risk for new HPV infections and consider the potential benefits of vaccination. Since the vaccine is most effective when given before exposure to HPV, its benefits may be reduced for this age group.
Read more about why it is important to get vaccinated here.
HPV-related cancers often don’t cause symptoms until they are advanced, serious, and difficult to treat.
CDC Recommended Vaccination Schedules
To ensure that your entire family is up to date on their vaccines, check out the following CDC recommended immunization schedules and talk to your healthcare provider.
HPV vaccination provides safe, effective, and long-lasting protection.
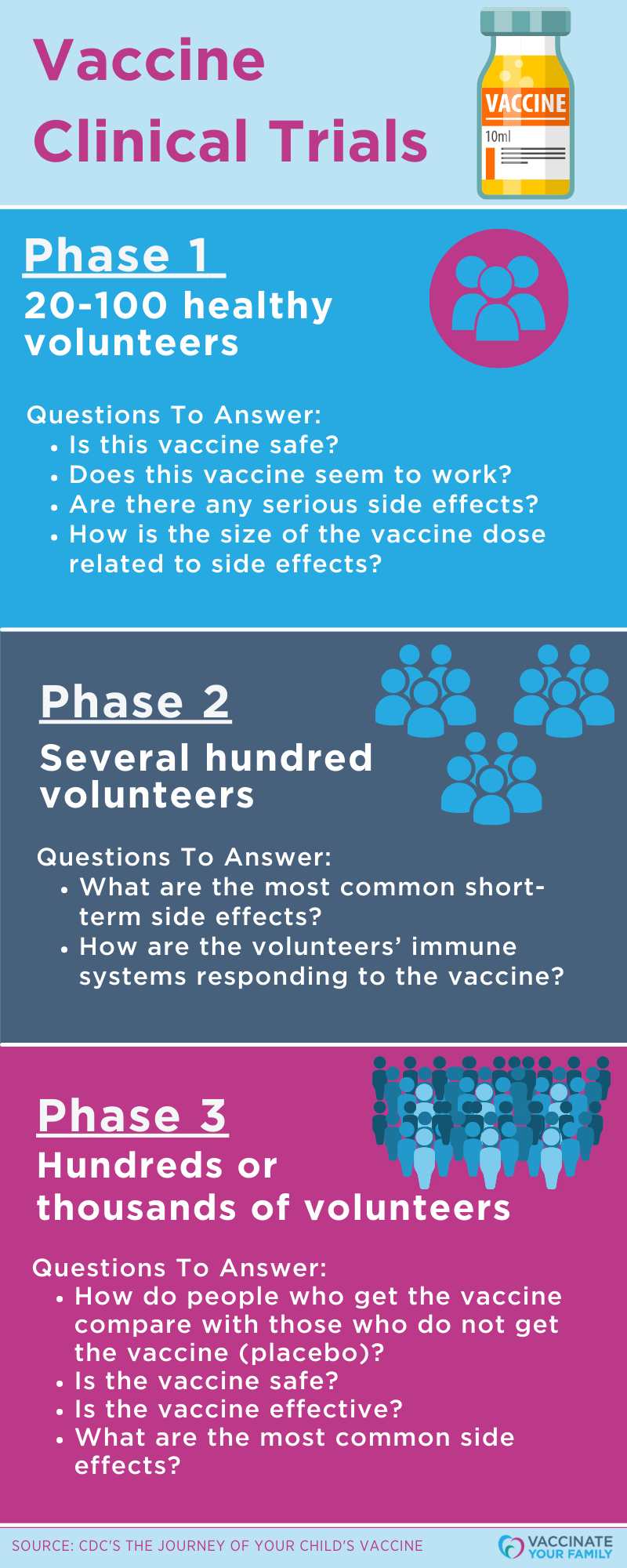
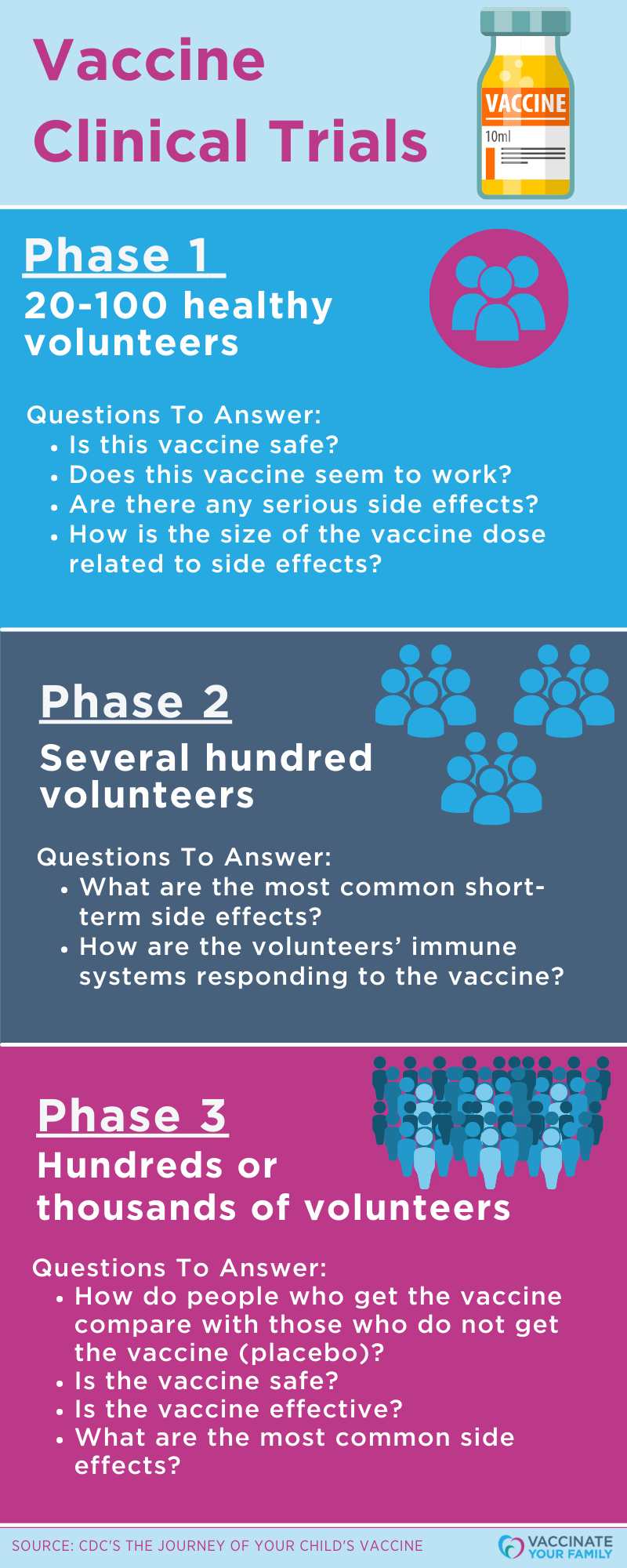
Numerous research studies have been conducted to make sure HPV vaccines are safe, both before and after the vaccines were approved/licensed and recommended for use in the U.S. Before HPV vaccines were licensed by the FDA for use in the U.S, they went through years of testing including clinical trials by thousands of people. After being licensed, the CDC and FDA have continued to monitor the safety of the HPV vaccines through the vaccine safety monitoring systems in the U.S. These included the Vaccine Adverse Event Reporting System (VAERS), Vaccine Safety Datalink (VSD), and the Clinical Immunization Safety Assessment (CISA).
Learn more about vaccine safety monitoring in the U.S.
Since the vaccine’s introduction in 2006, vaccine safety monitoring and studies conducted by CDC, FDA, and other organizations have documented an impressive safety record for HPV vaccines. There is no current evidence that HPV vaccines cause fertility problems in women.
As part of ongoing safety monitoring of HPV vaccines, CDC has reviewed reports of primary ovarian insufficiency (POI), also known as “premature menopause,” in the Vaccine Adverse Events Reporting System (VAERS) after both Gardasil 9 and Gardasil vaccination. CDC has also conducted additional safety research on the HPV vaccine in the Vaccine Safety Datalink (VSD). Learn more about safety research here.
Over 120 million doses of HPV vaccines have been distributed in the U.S. so far, and HPV vaccines continue to have an excellent safety record.
Like any vaccine or medicine, HPV vaccines can cause side effects, but the most common side effects are mild. They include pain, redness or swelling in the arm where the shot was given. Other side effects may include dizziness; fainting, nausea, and headache, which are often due to vaccine anxiety and fear. Severe allergic reactions are rare but can be life-threatening. The benefits of HPV vaccination far outweigh any potential risk of side effects.
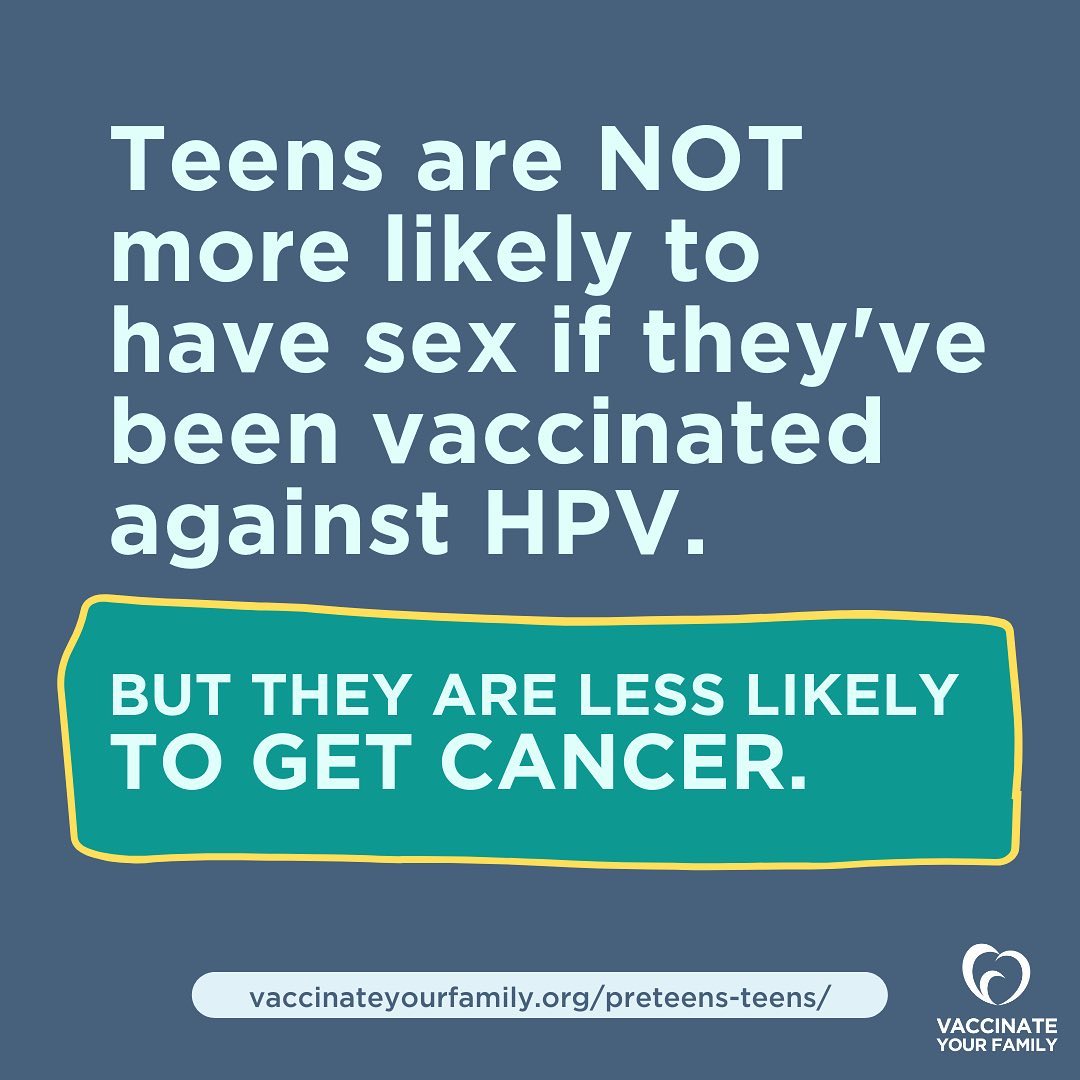
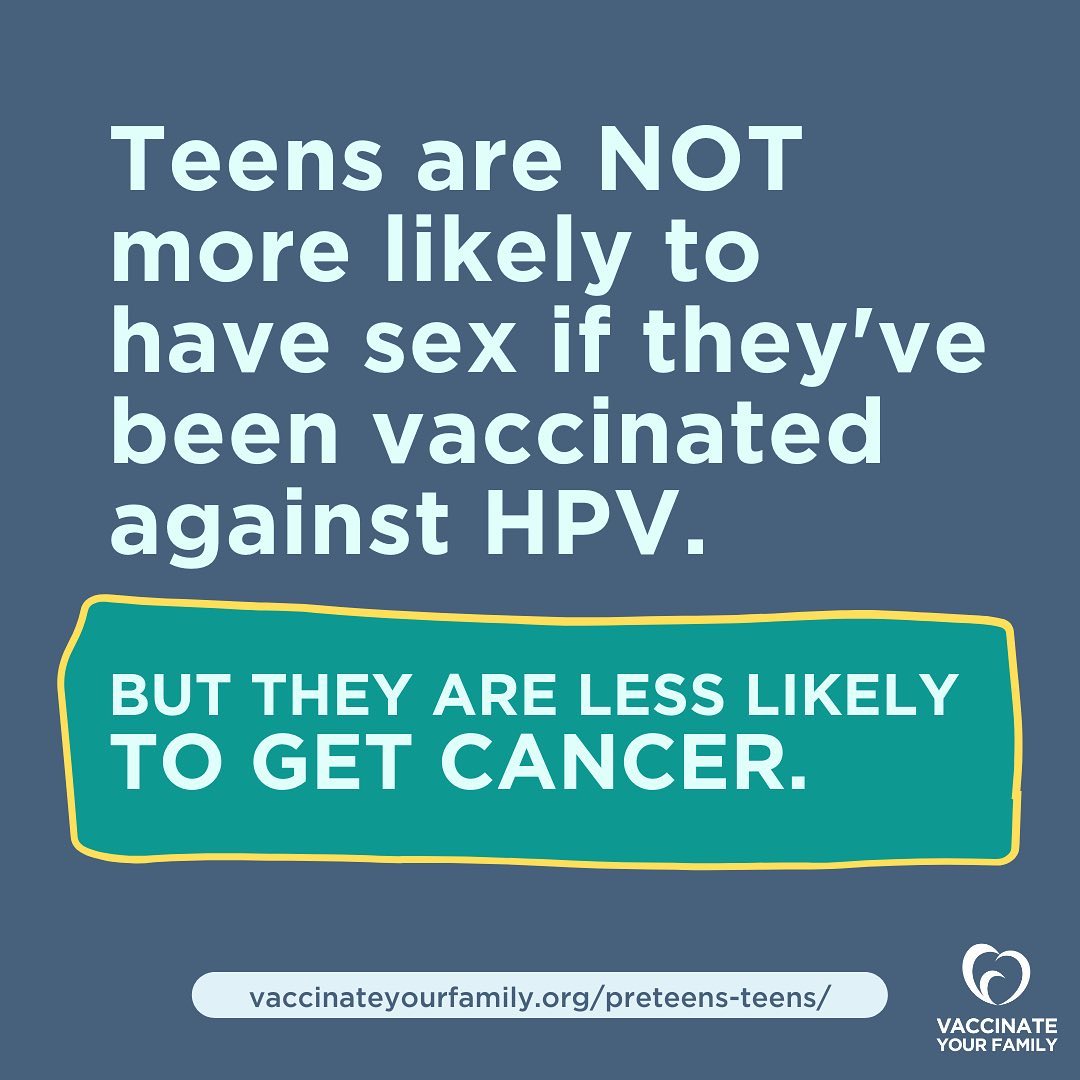
For the HPV vaccine to offer the best protection, it should be given before a child is exposed to HPV—before they begin any type of sexual activity. There is no reason to wait to vaccinate until your child reaches puberty or starts having sex.
Many parents may be surprised to learn that sexual intercourse is not required for HPV transmission. HPV can be spread through oral-genital contact, as well as hand-genital contact. A person can become infected with HPV during their first sexual encounter.